Around a year ago, 12-year-old Houssam suddenly lost consciousness and nearly fell into a coma. After being hospitalized, the boy was diagnosed with type 1 diabetes. But Houssam and his family live in Lebanon’s Bekaa valley, where there are very few treatment options for children living with the disease.
“The news really scared us,” said Mohammed, Houssam’s father. “We didn’t know that this disease could affect children. We had wrong perceptions about diabetes and how its treatment goes.” Houssam’s parents couldn’t afford the costly long-term treatment Houssam needed, so he was referred to Doctors Without Borders/Médecins Sans Frontières (MSF)—first to our pediatric ward at the Elias Hraoui Governmental Hospital in Zahle, where he was stabilized, then to a clinic in Aarsal for continuous diabetes care.
In Aarsal, MSF provides medical consultations, treatment, and health education. Houssam also received all the necessary tools to measure his blood sugar levels and receive insulin injections. Type 1 diabetes affects young people, who often have trouble adapting to life with an incurable chronic disease. One of the hardest things to adjust to is taking medication via injections.
In type 1 diabetes, the pancreas does not produce enough insulin, preventing blood sugar (glucose) from entering cells to for energy production. Treatment of the disease requires periodic monitoring of blood sugar levels, especially since children affected by type 1 diabetes are prone to sudden imbalances that can have serious complications and long-term side effects.
However, these risks don’t mean patients can’t still live normal lives with proper care, which is where MSF comes in. With disease management education for parents and children and regular medical follow-ups, patients like Houssam can continue to pursue their dreams.
“I dream of traveling to Sweden to study and become a doctor,” says Houssam. “I got used to living with the disease, and I am now able to keep it under control with the help of my parents and the support of the medical team. The most difficult thing about it is not being able to have French fries whenever I want and having to take insulin with needles."
Cutting down on needles
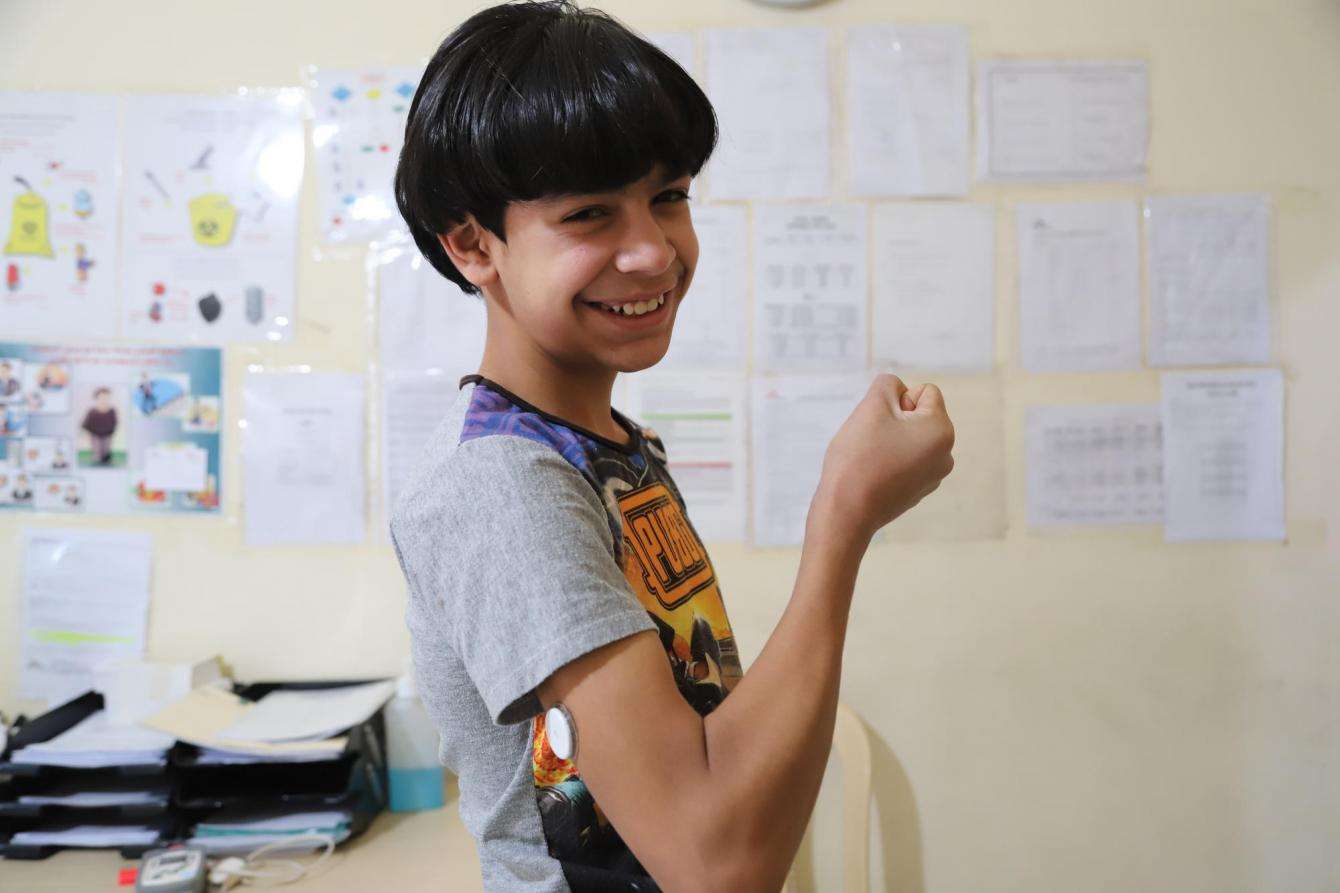
In mid-2019, MSF launched a new program for diabetes patients to cut down on the number of needles they have to use—and improve their adherence to treatment. Houssam and 79 other children under 15 years old receiving care for type 1 diabetes in the Bekaa valley and northern Lebanon now participate in the continuous glucose monitoring (CGM) program, in which patients wear a sensor on their arm that measures blood sugar levels.
The device is checked at specific times during the day and night to save and display glucose level data, allowing patients and parents to take immediate action and address sudden drops or spikes in sugar levels. This also allows the medical team to adjust the treatment program during the medical examination based on accurate data. And it means patients don’t have to prick their fingers every time they need to test their blood sugar.

Adapting to life with diabetes
In Shatila refugee camp, in southern Beirut, 12-year-old Cedra shares Houssam’s struggle with diabetes and the challenges of committing to a new diet, as she often wishes she could have sweets with her siblings and friends. Cedra uses another treatment technique provided by MSF, getting her insulin doses using an insulin pen. MSF provides the pen to more than 100 children in its clinics in Shatila camp, which is home to more than 10,000 refugees from Syria, Palestine, and other countries. MSF plans to expand the insulin pen program to its clinics in the Bekaa valley as well, which means Houssam will soon have access to the tool as well.
“We use the insulin pen with children and adolescents suffering from diabetes type 1, because it is more practical for them,” said Laura Rinchey, MSF’s project medical referent in southern Beirut. “Children or parents can adjust the insulin dosage with more precision—not to mention it is fast-acting. The objective behind this technique is to allow children to control their disease and manage their health on their own.” Health education and counseling teams also work closely with children and parents to help them adapt to life with diabetes.

Courage in the face of uncertainty
Without MSF’s free services, Houssam and Cedra would likely not be receiving quality care for their diabetes. Because they are refugees in Lebanon, Cedra's family doesn’t have much money and is unable to afford the insulin, monitoring device, strips, and insulin pens she needs without assistance. “I am sometimes unable to provide the healthy food recommended for my daughter, let alone the medication,” she said. “This worries me.”
Though diagnosis with type 1 diabetes comes as a shock to children and parents in Lebanon, MSF medical teams report that parents now have increased awareness of the disease, and are protecting their children from its psychological repercussions and physical complications. They also describe the courage of their young patients.




