Community engagement and affordable medicines have been key to saving lives in Khayelitsha and beyond, though the fight is not over yet
“No treatment, one thousand deaths per day,” said Dr. Eric Goemaere, who opened Doctors Without Borders/Médecins Sans Frontières’ (MSF) first HIV treatment program in South Africa in 2000 in Khayelitsha. “And worse, there’s paranoia about this disease.”
While this may sound familiar in the time of COVID-19, Dr. Goemaere is, instead, reflecting on what he saw in South Africa 20 years ago. That’s when the international medical humanitarian organization opened a small clinic in Khayelitsha, a township on the outskirts of Cape Town where many people reside in informal settlements.
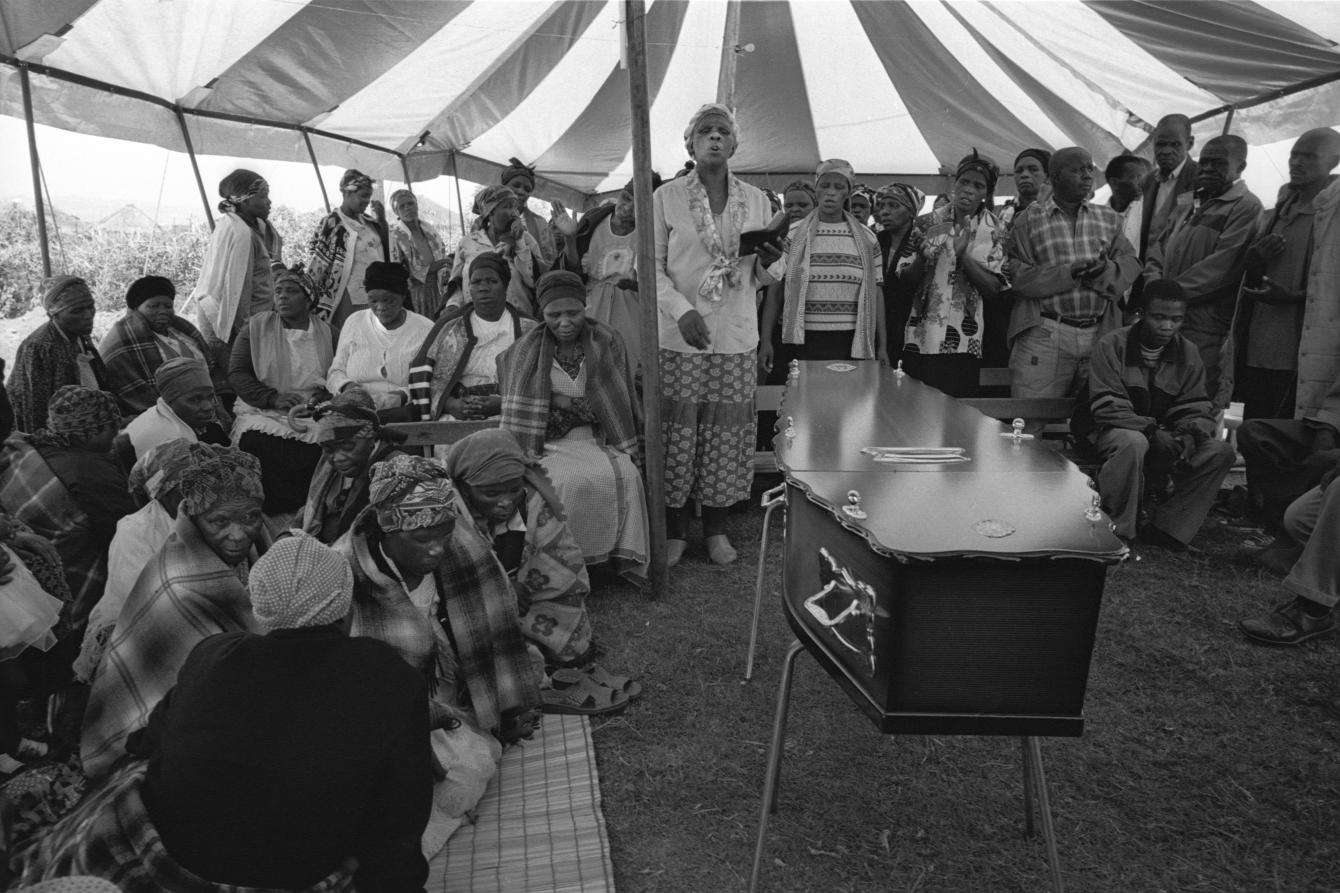
Twenty years ago, people with HIV in South Africa were arriving to clinics extremely sick, suffering from advanced HIV disease and fighting opportunistic infections such as tuberculosis (TB). Many of those who feared they had been infected but weren’t showing symptoms yet were hesitant to get tested because they didn’t want the stigma of the virus to interfere with getting jobs or forming relationships.
It was also a time when antiretroviral (ARV) medicines were priced out of reach. And leaders openly questioned how ARVs could work, even if they were affordable. Even the administrator of the United States Agency for International Development (USAID), Andrew Natsios, doubted it could, telling US lawmakers that USAID was opposed to giving Africans with HIV ARVs since they “do not know what watches and clocks are” and wouldn’t be able to take their medicines at the right time each day.
“The majority of people (coming to our clinic) could not walk anymore,” Dr. Goemaere said. “They were literally brought in wheelbarrows, or carried on the backs of their relatives. People were dying in the waiting room. While we were consulting behind the door, regularly we could hear people screaming, and this was a sign there was another death. And honestly, there was no single day without a death in the waiting room.”
But MSF’s clinic in Khayelitsha proved that treating and preventing the virus and disease was possible everywhere, not just in wealthy countries. Since opening this project—and subsequent programs including those to stop mother-to-child HIV transmission—MSF’s doctors, nurses, and non-medical staff have contributed to saving millions of lives in South Africa by providing direct care and advocating for affordable treatments for all.
Community-centered care
Khayelitsha’s success wouldn’t have been possible without working hand-in-hand with the community, listening to the needs of people living with and directly affected by HIV/AIDS—including local health care workers—and adapting interventions accordingly.
“I must applaud MSF, not only to see us as nurses or bedpan holders, but as people that can make decisions,” said Veliswa Labatala, an MSF nurse in Khayelitsha. “Because I think without the nurses—it was more like a nurse-driven project, of course under the supervision of doctors—maybe we wouldn’t have achieved what we have achieved today. (Our nurses) didn’t see themselves as only nurses, but they saw themselves as part of the community.”
Given the burden of HIV/AIDS in South Africa, many of MSF’s staff in Khayelitsha were personally affected, fueling their determination to tackle the epidemic.
“To run the clinics, (MSF) relied quite heavily on Xhosa-speaking nurses like myself,” said Nompumelelo Mantangana, a long-time MSF nurse in Khayelitsha. “We were more than nurses. Personally, I was motivated by the experience of seeing my brother living with HIV. One thing that bothered us all at the start was the fact that we could not provide ARVs for the mothers—it was all very well to save the children, but we were creating a whole generation of orphans.”
As for adapting interventions accordingly, one way MSF made it easier for people living with HIV to get and stick to their treatment regimens was by setting up ARV adherence clubs. Stable HIV-positive patients in these relatively small groups meet informally a few times per year in a medical facility or designated community location to get a couple-months’ worth of ARV supplies from a health care worker. This reduces the number of times per year they have to go to their clinic to pick up their medicines, which is welcomed by those who don’t have reliable transportation or who can’t afford to take time off work every week or month.
This particular community model of care has proven so successful it has been replicated in HIV projects and health facilities all over the world.
“So many of the different models of HIV care used worldwide were developed by MSF in Khayelitsha,” Mantangana said. “This included the first-ever ARV Adherence Clubs, which kept stable patients on ARVs by delivering efficient services in an environment of peer support. We could explain and discuss new developments in HIV care and get feedback from patients. It gave MSF the insight required to continue to develop ever-more patient-friendly interventions.”
By reducing viral load in people with HIV, ARV protects individuals from deadly opportunistic infections and protects public health by lowering the chances of transmission of the virus in the community.

Advocating for affordable treatment
In the early 2000s, access to ARVs to fight HIV/AIDS in low-resource settings like Khayelitsha was extremely limited because pharmaceutical corporations charged high prices and enforced patents that kept medicines out of reach. Patents prevented generic manufacturers from producing more affordable versions of these lifesaving medicines.
While the wealthiest people could afford the thousands of dollars pharmaceutical corporations charged for these medicines, most patients and treatment providers couldn’t and were forced to go without. At this time, ARVs were sold for more than $10,000 per person per year.
MSF staff, people living with HIV, and activists like those with Treatment Action Campaign (TAC)—an organization with which MSF worked closely to demand affordable ARVs in South Africa—began speaking out, which led the government to agree in 2004 to start providing ARVs for people with HIV/AIDS. This pressure had a ripple effect across the globe, eventually leading to lower prices everywhere.
Since then, ARV prices have dropped by more than 99 percent, primarily because of the availability of generic medicines.
“I want to talk about what makes MSF different,” said Nathan Geffen, a leader of TAC. “I don’t think (MSF staff) ever thought of themselves as charity workers. What MSF was doing with TAC at the forefront of the struggle was setting an example to show that we can treat a few thousand people. But that’s not our aim. The aim was to get millions of people onto treatment. That’s politics, and that’s what political activism achieves. That’s what separates MSF from so many other similar service delivery organizations around the world.”
From 2000 to 2019, the percentage of people who had access to ARVs went from zero to 71 percent, making South Africa the largest ARV program in the world with more than five million people receiving treatment.
The fight continues
While fewer people are dying from HIV in South Africa today—72,000 in 2019 compared to 150,000 in 2000—the virus is still one of the leading causes of death in the country.
To drive these numbers down even further, anyone who tests positive for HIV should be immediately put on treatment rather than having to wait until the next appointment, which that person may or may not attend. This “test and treat” approach has proven very successful but is still not the standard everywhere.
Care shouldn’t end there; people living with HIV need stable support and access to medicines after the diagnosis. We often see people stop taking their treatments, which can cause a person’s condition to deteriorate and also cause them to “fail” treatment, which means that a particular medication will no longer work for them because they’ve become resistant to it. Oftentimes this forces people to take second- and third-line ARVs, which can still be quite expensive.
Several other obstacles remain, such as a lack of easy-to-use, along with point-of-care diagnostic options for HIV/AIDS and common co-infections, especially in the low-resource and remote settings where MSF works. This is even more true for people with advanced HIV, which is a stage where people are especially at-risk of contracting an opportunistic infection like TB, meningitis, cryptococcal meningitis, and severe bacterial infections.
To prevent HIV/AIDS-related deaths, it’s critical that medicines for people with advanced HIV are more widely available, as well as medicines to fight opportunistic infections. TB and drug-resistant TB (DR-TB) medicines, for example, are often priced out of reach or simply not registered in countries—including high-burden TB countries—because companies don’t see the profit in doing so. Worldwide, TB is the leading cause of death of HIV-positive people in low-resource settings, causing up to 50 percent of deaths among HIV-positive people.
“The ‘access to medicines’ fight was a very important fight that happened 20 years ago to say we want access to affordable medicines,” said Nathan Ford, former medical director for MSF's Access Campaign. “But that fight continues 20 years later as well. We’re always looking around the corner at how to further improve the treatment we have.”
Additionally, it is critical that actors like The Global Fund to Fight AIDS, Tuberculosis and Malaria, as well as the US President's Emergency Plan for AIDS Relief (PEPFAR) continue to support countries in their fight to end HIV/AIDS. The global health community has made great strides on HIV throughout the past 20 years, but failing to fund countries’ efforts to carry out health programs now could undo that progress.


